Type 2 diabetes is a chronic condition that affects how your body processes blood sugar (glucose). With over 37 million Americans living with diabetes—90-95% of whom have type 2—this condition represents one of today’s most significant health challenges. When you have type 2 diabetes, your body either doesn’t produce enough insulin or becomes resistant to its effects, resulting in high blood sugar levels that can damage organs and systems throughout your body. This comprehensive guide explores the causes, symptoms, diagnosis methods, and management strategies to help you understand and effectively address this condition.
What Is Type 2 Diabetes?
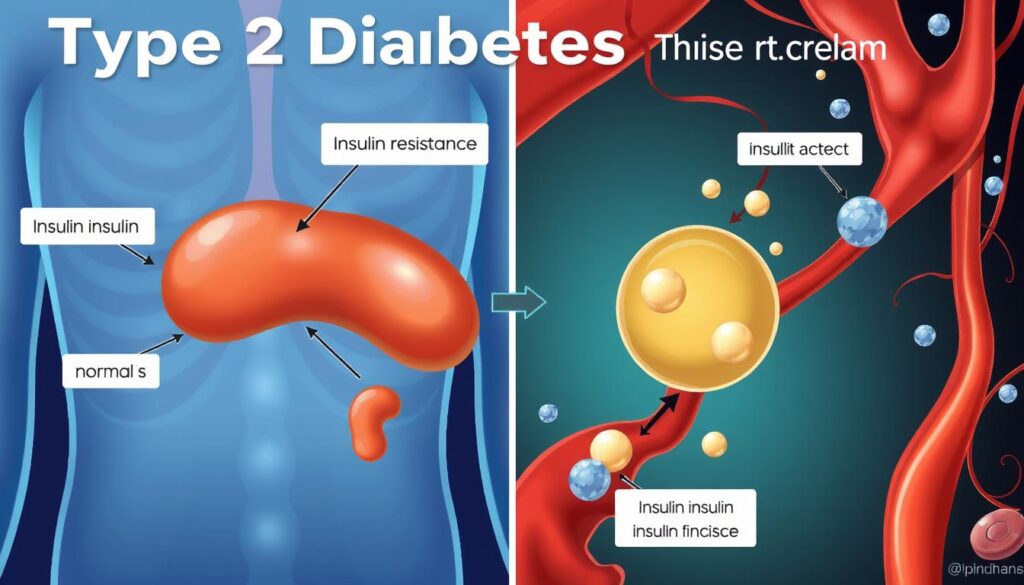
Type 2 diabetes occurs when cells become resistant to insulin or when the pancreas doesn’t produce enough insulin.
Type 2 diabetes is a metabolic disorder characterized by high blood sugar levels (hyperglycemia) resulting from insulin resistance and relative insulin deficiency. Unlike type 1 diabetes, which is an autoimmune condition where the pancreas produces little to no insulin, type 2 diabetes develops gradually as your body’s cells become less responsive to insulin.
Healthy blood sugar levels typically range from 70 to 99 milligrams per deciliter (mg/dL). In people with undiagnosed type 2 diabetes, these levels are often 126 mg/dL or higher. This persistent elevation in blood glucose can lead to serious health complications if left untreated.
Researchers estimate that type 2 diabetes affects approximately 6.3% of the world’s population, making it the ninth leading cause of death globally. While it most commonly affects adults over 45, increasing numbers of younger adults and even children are developing the condition, largely due to rising obesity rates and sedentary lifestyles.
Concerned About Your Diabetes Risk?
Take our free risk assessment quiz to understand your likelihood of developing type 2 diabetes and receive personalized prevention recommendations.
Causes and Risk Factors of Type 2 Diabetes

The development of type 2 diabetes involves a complex interplay of genetic, lifestyle, and environmental factors. The primary mechanism behind this condition is insulin resistance, where cells in your muscles, fat, and liver don’t respond properly to insulin, forcing your pancreas to produce more insulin to overcome rising blood glucose levels.
Key Contributors to Insulin Resistance
- Excess body fat: Particularly visceral fat (fat around your organs) increases inflammation and hormonal imbalances that promote insulin resistance.
- Physical inactivity: Regular exercise helps your body use insulin more effectively. Lack of activity contributes to insulin resistance.
- Dietary factors: Frequent consumption of highly processed foods, refined carbohydrates, and saturated fats can impair insulin sensitivity.
- Genetics: Your lifetime risk increases to 40% if one parent has type 2 diabetes and 70% if both parents have it.
- Chronic stress and poor sleep: Both can affect hormone regulation and contribute to insulin resistance.
Who’s at Risk?
Non-Modifiable Risk Factors
- Age: Risk increases after age 45
- Family history: Having a parent or sibling with the condition
- Ethnicity: Higher risk in Black, Hispanic, Native American, Asian American, and Pacific Islander populations
- History of gestational diabetes: Increases future risk
- Polycystic ovarian syndrome (PCOS): Associated with insulin resistance
Modifiable Risk Factors
- Overweight or obesity: Especially with a BMI greater than 25
- Sedentary lifestyle: Physical activity less than three times weekly
- Poor diet: High in processed foods and added sugars
- Smoking: Increases inflammation and insulin resistance
- Prediabetes: Blood sugar levels higher than normal but not yet diabetic
Research has identified at least 150 DNA variations linked to type 2 diabetes risk. Some directly affect insulin production and resistance, while others influence weight gain tendencies. These genetic factors interact with lifestyle choices to determine your overall risk.
Symptoms and Diagnosis of Type 2 Diabetes

Common Symptoms
Type 2 diabetes often develops gradually, with symptoms appearing slowly over time. Some people may have the condition for years before noticing symptoms. When they do appear, common signs include:
Early Symptoms
- Increased thirst (polydipsia)
- Frequent urination
- Unusual hunger
- Unexplained fatigue
Progressive Symptoms
- Blurred vision
- Slow-healing cuts or sores
- Recurring infections
- Unexplained weight loss
Advanced Symptoms
- Tingling or numbness in extremities
- Dark patches of skin (acanthosis nigricans)
- Frequent yeast infections
- Dry, itchy skin
When to See a Doctor: If you experience several of these symptoms, especially increased thirst, frequent urination, and unexplained fatigue, consult a healthcare provider promptly. Early diagnosis can prevent serious complications.
Diagnostic Tests for Type 2 Diabetes
Healthcare providers use several blood tests to diagnose type 2 diabetes:
| Test | Procedure | Diabetes Diagnosis Threshold | Prediabetes Range |
| Fasting Plasma Glucose (FPG) | Blood test after 8-hour fast | ≥126 mg/dL | 100-125 mg/dL |
| A1C Test | Measures average blood sugar over 2-3 months | ≥6.5% | 5.7-6.4% |
| Oral Glucose Tolerance Test (OGTT) | Blood test 2 hours after consuming glucose solution | ≥200 mg/dL | 140-199 mg/dL |
| Random Plasma Glucose Test | Blood test at any time of day | ≥200 mg/dL with symptoms | N/A |
Typically, a diagnosis requires at least two abnormal test results from the same sample or from two separate test samples. If you’re diagnosed with type 2 diabetes, your healthcare provider may recommend additional tests to check for complications or coexisting conditions.
Know Your Symptoms
Download our comprehensive Type 2 Diabetes Symptom Checklist to track your symptoms and share with your healthcare provider.
Management Strategies for Type 2 Diabetes

Managing type 2 diabetes effectively requires a comprehensive approach that combines lifestyle modifications, regular monitoring, and often medication. The goal is to keep your blood sugar levels within a target range to prevent or delay complications.
Lifestyle Modifications
Nutrition for Type 2 Diabetes
There’s no one-size-fits-all diet for diabetes, but certain nutritional principles can help manage blood sugar levels:
Foods to Emphasize
- Non-starchy vegetables: Broccoli, spinach, peppers
- Lean proteins: Chicken, fish, tofu, eggs
- Healthy fats: Avocados, nuts, olive oil
- Complex carbohydrates: Whole grains, legumes
- Fiber-rich foods: Berries, beans, oats
Foods to Limit
- Refined carbohydrates: White bread, pastries
- Added sugars: Sodas, candy, desserts
- Processed meats: Bacon, sausage, deli meats
- Trans and saturated fats: Fried foods, fatty cuts of meat
- Alcohol: Can affect blood sugar unpredictably
Working with a registered dietitian who specializes in diabetes can help you develop a personalized meal plan that fits your preferences, cultural background, and specific health needs.
Physical Activity
Regular exercise is crucial for managing type 2 diabetes as it:
- Improves insulin sensitivity, allowing your body to use insulin more effectively
- Helps maintain a healthy weight
- Lowers blood pressure and cholesterol levels
- Reduces stress and improves overall well-being
The American Diabetes Association recommends aiming for at least 150 minutes of moderate-intensity aerobic activity weekly, spread over at least 3 days, with no more than 2 consecutive days without activity. Strength training at least twice weekly is also beneficial.

Blood Sugar Monitoring
Regular monitoring helps you understand how food, activity, stress, and medication affect your blood sugar levels. There are two main approaches:
Self-Monitoring with Glucose Meter
- Involves pricking your finger to obtain a blood sample
- Provides immediate readings of current blood sugar levels
- Frequency depends on your treatment plan and provider recommendations
Continuous Glucose Monitoring (CGM)
- Uses a sensor inserted under the skin to measure glucose levels
- Provides readings every few minutes throughout the day and night
- Shows trends and patterns in blood sugar fluctuations
Medications for Type 2 Diabetes
If lifestyle changes aren’t sufficient to manage your blood sugar levels, your healthcare provider may prescribe medication. Common options include:
| Medication Class | How It Works | Common Examples | Considerations |
| Metformin (Biguanides) | Reduces glucose production by the liver and improves insulin sensitivity | Glucophage, Fortamet, Glumetza | Usually first-line treatment; may cause digestive side effects initially |
| Sulfonylureas | Stimulates pancreas to release more insulin | Glipizide, Glyburide, Glimepiride | May cause hypoglycemia (low blood sugar) |
| DPP-4 Inhibitors | Helps body continue to make insulin and reduce glucose production | Sitagliptin, Saxagliptin, Linagliptin | Less likely to cause hypoglycemia; may cause joint pain |
| SGLT2 Inhibitors | Prevents kidneys from reabsorbing glucose, increasing glucose excretion | Empagliflozin, Canagliflozin, Dapagliflozin | May provide cardiovascular benefits; increases risk of genital infections |
| GLP-1 Receptor Agonists | Slows digestion, reduces glucose production, increases insulin production | Semaglutide, Liraglutide, Exenatide | Injectable; may aid weight loss; may cause nausea initially |
| Insulin | Replaces or supplements body’s natural insulin | Long-acting (glargine), Rapid-acting (lispro) | Used when other medications aren’t sufficient; requires careful monitoring |
Track Your Blood Sugar Effectively
Download our Blood Sugar Tracking Template to monitor your levels and identify patterns that affect your diabetes management.
Complications of Type 2 Diabetes

Persistently high blood sugar levels can damage blood vessels and nerves throughout your body, leading to various complications. Managing your diabetes effectively can significantly reduce your risk of developing these problems.
Major Complications
Cardiovascular Complications
- Heart disease: 2-4x higher risk
- Stroke: 1.5x higher risk
- Peripheral artery disease: Reduced blood flow to limbs
- High blood pressure: Common comorbidity
Microvascular Complications
- Diabetic retinopathy: Leading cause of blindness
- Diabetic nephropathy: Kidney damage or failure
- Diabetic neuropathy: Nerve damage causing pain, tingling
- Foot problems: Ulcers, infections, amputation risk
Other Complications
- Skin conditions: Bacterial and fungal infections
- Hearing impairment: Higher prevalence
- Cognitive decline: Increased dementia risk
- Depression: 2-3x more common
Medical Emergency: Hyperosmolar hyperglycemic state (HHS) is a life-threatening complication of extremely high blood sugar. Symptoms include extreme thirst, confusion, vision changes, and weakness. Seek immediate medical attention if these symptoms occur.
Speak With a Diabetes Specialist
Don’t face diabetes complications alone. Connect with a qualified healthcare provider who specializes in diabetes care.
Prevention of Type 2 Diabetes

If you have risk factors for type 2 diabetes, making targeted lifestyle changes can significantly reduce your chances of developing the condition. Research shows that people with prediabetes can reduce their risk by 58% through lifestyle modifications.
Effective Prevention Strategies
Weight Management
Losing just 5-7% of your body weight can make a substantial difference. For someone weighing 200 pounds, that’s just 10-14 pounds.
- Focus on sustainable weight loss approaches
- Set realistic goals with your healthcare provider
- Consider working with a registered dietitian
Regular Physical Activity
Aim for at least 150 minutes of moderate-intensity exercise weekly.
- Start slowly and gradually increase intensity
- Include both aerobic and strength training exercises
- Find activities you enjoy to maintain consistency
Healthy Eating Patterns
Focus on a balanced diet rich in whole foods.
- Emphasize vegetables, fruits, and whole grains
- Choose lean proteins and healthy fats
- Limit processed foods, refined carbs, and added sugars
- Practice portion control
Lifestyle Habits
Other factors that can reduce your risk:
- Quit smoking
- Limit alcohol consumption
- Manage stress through mindfulness, meditation, or other techniques
- Prioritize quality sleep (7-8 hours nightly)
- Stay hydrated with water instead of sugary beverages
“Prevention is particularly important for those with prediabetes. With appropriate lifestyle changes, many people can delay or even prevent the progression to type 2 diabetes.”
Assess Your Diabetes Risk
Take our comprehensive risk assessment to understand your personal risk factors and receive a customized prevention plan.
Latest Research and Advancements

The field of diabetes research continues to evolve rapidly, with promising developments in treatment approaches, technology, and understanding of the disease mechanisms. Here are some notable recent advancements:
Breakthrough Treatments
GLP-1 Receptor Agonists
These medications, originally developed for diabetes management, have shown remarkable effectiveness for both blood sugar control and weight management. Recent studies have demonstrated that medications like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro) can help people lose significant weight (15-20% of body weight) while improving blood sugar control.
Dual GIP/GLP-1 Receptor Agonists
Newer medications like tirzepatide target both GLP-1 and GIP receptors, potentially offering superior glucose control and weight loss compared to single-target therapies.
Technological Innovations
Advanced Glucose Monitoring
- Continuous glucose monitoring (CGM) systems are becoming more accurate, smaller, and more affordable
- Some newer systems eliminate the need for fingerstick calibration
- Integration with smartphones allows for real-time data sharing with healthcare providers
Artificial Pancreas Systems
- Closed-loop systems that automatically adjust insulin delivery based on CGM readings
- Reduce the burden of diabetes management decisions
- Improve time in target blood sugar range
Emerging Research Areas

Precision Medicine
- Tailoring treatments based on individual genetic profiles
- Identifying subtypes of type 2 diabetes for targeted therapies
- Predicting medication response based on biomarkers
Gut Microbiome
- Exploring connections between gut bacteria and insulin sensitivity
- Investigating probiotics and prebiotics as potential interventions
- Understanding how diet affects microbiome composition
Digital Health Solutions
- AI-powered decision support tools
- Mobile apps for comprehensive diabetes management
- Telehealth platforms for remote monitoring and care
While these advancements show promise, it’s important to work with your healthcare provider to determine which approaches are appropriate for your specific situation. Not all new treatments are suitable for everyone with type 2 diabetes.
Stay Updated on Diabetes Research
Subscribe to our newsletter to receive the latest updates on type 2 diabetes research, treatments, and management strategies.
Living Well with Type 2 Diabetes

While type 2 diabetes is a chronic condition that requires ongoing management, many people live full, active lives with the disease. Developing a comprehensive self-care routine and building a strong support network are key to thriving with diabetes.
Building Your Diabetes Management Team
Effective diabetes care typically involves multiple healthcare professionals:
Primary Care Providers
- Primary care physician
- Endocrinologist
- Nurse practitioner
Specialists
- Certified diabetes educator
- Registered dietitian
- Pharmacist
Allied Health Professionals
- Ophthalmologist
- Podiatrist
- Mental health provider
Daily Management Strategies
Developing Routines
- Establish consistent meal times
- Schedule regular physical activity
- Create medication reminders
- Plan for regular blood sugar checks
Problem-Solving Skills
- Learn to recognize and treat low blood sugar
- Develop sick-day management plans
- Prepare for travel and special occasions
- Adjust for changes in routine
Emotional Well-being
Living with a chronic condition can take a toll on mental health. People with diabetes are 2-3 times more likely to experience depression than those without the condition. Strategies to support emotional well-being include:
- Acknowledging the emotional aspects of diabetes management
- Connecting with diabetes support groups (online or in-person)
- Practicing stress-reduction techniques like meditation or deep breathing
- Seeking professional mental health support when needed
- Setting realistic goals and celebrating small victories

“Diabetes distress—the emotional burden of managing a demanding chronic disease—affects up to 45% of people with diabetes. Recognizing and addressing these feelings is an essential part of comprehensive diabetes care.”
Taking Control of Type 2 Diabetes
Type 2 diabetes presents significant challenges, but with proper management, you can lead a healthy, fulfilling life. By understanding the condition, working closely with healthcare providers, making sustainable lifestyle changes, and staying informed about the latest advancements, you can effectively manage your blood sugar levels and reduce your risk of complications.
Remember that diabetes management is a marathon, not a sprint. Small, consistent actions taken daily have a greater impact than occasional major efforts. Be patient with yourself, celebrate your progress, and don’t hesitate to reach out for support when needed.
Whether you’re newly diagnosed, at risk for developing type 2 diabetes, or supporting a loved one with the condition, knowledge is power. Use the information and resources provided in this guide as a starting point for your diabetes management journey, and continue to seek out reliable, up-to-date information from trusted healthcare providers and organizations.
Take the Next Step in Your Diabetes Journey
Download our comprehensive Type 2 Diabetes Management Guide for practical tips, tracking tools, and resources to help you take control of your health.
Frequently Asked Questions About Type 2 Diabetes
Can type 2 diabetes be reversed?
While type 2 diabetes is generally considered a chronic, progressive condition, some people can achieve remission through significant lifestyle changes, particularly substantial weight loss. Remission means maintaining normal blood sugar levels without medication, but it doesn’t mean the diabetes is “cured.” The underlying genetic predisposition remains, and the condition can return if triggering factors reappear. Bariatric surgery has also been shown to induce remission in some cases.
What’s the difference between type 1 and type 2 diabetes?
Type 1 diabetes is an autoimmune condition where the body attacks and destroys insulin-producing cells in the pancreas, resulting in little to no insulin production. It typically develops in childhood or adolescence and requires insulin therapy for life. Type 2 diabetes involves insulin resistance and relative insulin deficiency. It develops gradually, usually in adults (though increasingly in younger people), and can often be managed with lifestyle changes and oral medications before insulin might be needed.
How often should I check my blood sugar if I have type 2 diabetes?
The frequency of blood sugar monitoring varies based on your treatment plan, medication regimen, and how well your diabetes is controlled. Those taking insulin typically need to check more frequently than those managing with lifestyle or oral medications. Your healthcare provider will recommend a monitoring schedule tailored to your specific situation. With the increasing availability of continuous glucose monitoring systems, monitoring patterns may be changing for many people with type 2 diabetes.
Can I still eat carbohydrates if I have type 2 diabetes?
Yes, carbohydrates can still be part of your diet with type 2 diabetes. The key is focusing on the quality, quantity, and distribution of carbs throughout the day. Complex carbohydrates from whole grains, legumes, fruits, and vegetables are preferable to refined carbs and added sugars. Working with a registered dietitian can help you develop a personalized meal plan that includes appropriate carbohydrates while maintaining good blood sugar control.
Is type 2 diabetes genetic or lifestyle-related?
Type 2 diabetes results from a complex interaction between genetic and environmental factors. Having a family history significantly increases your risk, indicating a strong genetic component. However, lifestyle factors like diet, physical activity, and weight play crucial roles in whether those genetic predispositions are expressed. This explains why type 2 diabetes can often be prevented or delayed through lifestyle modifications, even in those with genetic risk factors.


Pingback: Why Mochi Health Is Changing the Game in Personalized Wellness